Infertility problems relating to male factor accounts for approximately 40% of all couples having difficulties conceiving. It is therefore critical that a complete and thorough examination of the male is performed.
Due to the fact that the examination of a male is relatively non-invasive, this is often one of the first tests performed in investigating the cause of infertility.
The test used to assess male fertility is done via a semen analysis and sperm antibodies; it measures the key parameters of semen known to impact fertility. Laboratories do vary in their ability to provide an accurate semen analysis and as such it is recommended that the test is performed by a fertility scientist with extensive experience in semen evaluation and will follow the guidelines and assessment of the World Health Organisation (WHO).
Preparing For The Test
The test requires a referral from either a GP or fertility specialist. Semen analysis test can be done at major of pathology centre (ie QML). There is a cost associated to the test. The results will be sent back to your referring doctor/specialist, please follow up directly with the referring doctor.
In order to obtain an accurate result, it is important to follow the instructions below when preparing for the test:
- There MUST be a period of abstinence from sexual activity for between 2-7 days. It is a very common misunderstanding that sperm quality improves if it is ‘stored up’. However this is not the case, sperm are constantly produced by the testes and stored within a long tubular structure called the epididymis. During ejaculation, sperm are flushed from the epididymis and fresh sperm refill within about 2-3 days. Therefore testing less than 2 days may result in a decreased concentration (or sperm count). Whilst testing past 7 days can result in decreased motility (sperm moving in a forward direction). This is because sperm cells have a limited lifespan of approximately 3 weeks maximum inside the testes. When ejaculation is infrequent, sperm cells start to die. DNA fragmentation is also reduced via frequent ejaculation (i.e. every couple of days).
- The sample should be collected via masturbation. Collecting a sample can be a little uncomfortable and daunting for some men. Masturbation is the preferred collection method to ensure that a sample is neither contaminated nor compromised during collection. Condoms which are purchased from the chemist etc. have a toxic substance which are designed to kill sperm and therefore will affect the viability of sperm. There are however, some other options available to men experiencing difficulty collecting a sample via masturbation (e.g. non-toxic collection kit), which should be discussed with a scientist. As such this will assist in an accurate result being reported, which is reflective of a patient’s sample.
- The whole sample must be collected. In order to get a result which is reflective of a patient’s ‘normal’ sample, ideally the whole sample is collected. In the case where the whole sample is not collected in the specimen container, it is essential that you inform the fertility scientist. This is because depending on the portion of the sample missed, this could impact your result. Generally speaking the sperm-rich part of the ejaculate is in the first portion (therefore if this portion is missed, it may yield a low concentration). Therefore if the entire sample is not collected it may impact the result of the semen analysis and as such your referring doctor may suggest repeating the test.
- Collection of the sample MUST be in a suitable collection container. This is particularly important as an inappropriate specimen container can make the results invalid; due to possible toxicity of the collection container. You can obtain a semen container from a QML or Sullivan Nicolaides pathology centre or chemist.
- The sample must be assessed within one (1) hour of production. It is essential that the sample is delivered to the pathology centre within 1 hour of production. This is because although the seminal plasma is what makes the sperm motile initially upon ejaculation, the longer that the sperm remains in the seminal plasma the more compromised the sample becomes and a decrease in motility will occur.
- Keep the sample at room/body temperature during transportation to the pathology centre. The sample can be kept either at room temperature or body temperature during transportation to the pathology centre for assessment. It is essential not to heat or cool the sperm; both of these will have a detrimental effect on the sperm and impact the result. Ensure that the lid of the container is tightly secured and wrap the container in aluminium foil.
Factors That Can Affect Sperm Production
There are a number of factors that can affect the sperm production process and therefore impact the results of the semen analysis. These include:
- Smoking/Nicotine
- Recreational drugs
- Excessive alcohol (binge drinking)
- Prolonged exposure to chemicals (such as heavy metals and pesticides) or radiation
- Illness or infections in the genital tract – especially fevers or mumps
- Exogenous testosterone
- Age (decline >40 yrs)
- BMI (>30kg/m2)
- Caffeine intake
- Some antibiotics
Therefore, it is important to discuss anything of concern with your referring doctor or specialist.
Semen Analysis Results – What do they mean?
The results of the semen analysis will be discussed with you by your referring doctor, and will help determine the type of treatment most suitable to your needs. It is important to remember that if a repeat semen analysis is requested, please allow 3 months to elapse since the initial sample before the repeat is scheduled. This is because the length of the sperm production cycle is roughly 72 days.
The table below shows the most important parameters that are assessed during the semen analysis and the normal ranges as stipulated by the WHO.
| Semen Parameter | Normal Range |
|---|---|
| Volume | ≥ 1.5mL |
| Sperm Concentration | ≥ 15 million/mL |
| Progressive Motility | ≥ 32% with forward progression |
| Sperm Morphology (shape) | ≥ 4% for natural conception≥ 2% for assisted conception |
| Teratozoospermia Index (TZI) | ≤ 1.99 |
| Antisperm Antibodies | <50% sperm bound |
When results are outside the normal ranges (as defined in the above table), the following terms are used to describe the findings:
- Asthenozoospermia – reduced number of motile sperm
- Azoospermia – no sperm present in the ejaculate
- Oligospermia – reduced number of sperm in the sample
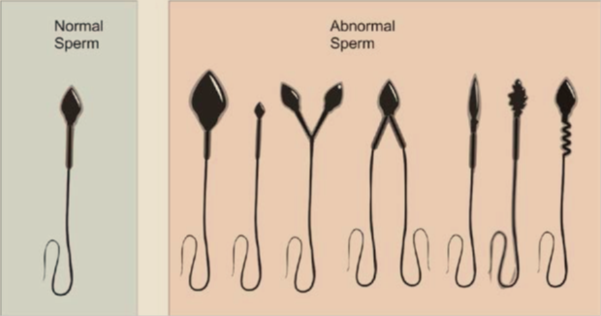
- Teratozoospermia – reduced number of normal shaped sperm
What Can You Do To Improve Semen Parameters?
The sperm production cycle is 72 days and as such, it is important to remember that what you were doing roughly 3 months ago can affect your semen parameters. Therefore if there is anything that you feel may have compromised the sample that you provided for analysis, please inform your referring doctor.
Lifestyle factors such as those listed above, are the main factors which contribute to poor semen parameters. However it is also important to realise that the semen analysis only examines the external appearance of the sample (i.e. number of sperm, movement and shape of the sperm). Even though these parameters can appear normal, the internal DNA structure of the sperm is not examined through this test. Therefore to assist with this DNA component, there are a couple of tricks to try:
- Although frequent ejaculation may reduce sperm concentration, it can assist with DNA fragmentation and is seen as an advantage for those patients who experience a higher-than-expected decline in embryos between days 3 and 5.
- Use of Menevit (which is a supplement formulated to maintain sperm health) or similar can assist in improving sperm concentration and DNA fragmentation.
Treatment Options
Your history and the results of the semen analysis will help your specialist determine the type of treatment that will suit your situation. Below are the different treatment options which may be recommended:
- Intrauterine Insemination (IUI) is generally recommended when the results of the semen analysis are normal. With this treatment, the motile sperm are separated, concentrated and inseminated into the uterus.
- In Vitro Fertilisation (IVF) is recommended for mild/moderate male factor infertility. With this treatment, the motile sperm are separated, concentrated and placed into a dish with the eggs collected at time of pick up.
- Intracytoplasmic Sperm Injection (ICSI) is recommended for severe male factor infertility. This technique is similar to IVF, as the sperm are processed in the same way. However, the procedure involves injecting a single sperm directly into the centre of the egg.
For further information please either phone 07 5478 2482 or email us at enquires@fssc.com.au.