Vitrification (or freezing) is a technology used for freezing eggs and is available at Fertility Solutions. While human sperm and embryos have been successfully frozen for decades and are considered routine and consistent technologies, human egg freezing is still a relatively new technique. As a newer technology it is too early to give the precise success rates of achieving a pregnancy and live birth from eggs that have been frozen, thawed and then fertilised. It has been suggested that the freezing and thawing methods may disrupt some of the components within the egg and therefore increase the potential for chromosome abnormalities in some of the resulting embryos produced from this procedure.
The goal of egg freezing is to attempt to preserve some fertility in women at risk of declining fertility. It is not a guarantee that a pregnancy or baby will result from the use of this technology.
Female Age & Fertility
It is important to know that a woman’s fertility is at its peak at around 27 and slowly declines from this point until menopause. There is a significant decline in a woman’s fertility from around 35 which becomes even more significant from 38 onwards – by the age of 40 approximately 90% of eggs produced by a woman are chromosomally abnormal and unlikely to result is a viable pregnancy.
Unlike a woman who continues to age, the eggs that have been frozen when she was 32 stay the same age that they were when they were frozen. This means that a woman freezing her eggs at 32 who then wants a baby at 40, has a much higher chance of having a healthy pregnancy and baby using her 32-year-old frozen eggs than she would if she were to try with her own 40-year-old eggs.
Who May Benefit?
Women who are faced with the following may find egg freezing suitable for them:
• Women who are under the age of 35 years who would like to or need to delay family commencement.
• Treatment of medical conditions or serious illness that may impact a woman’s fertility such as chemotherapy.
• Individuals wishing to preserve their fertility prior to gender reassignment.
The use of egg freezing therefore makes it possible for women to pursue careers and relationships or undergo lifesaving treatments, with the chance of a future successful pregnancy.
What Is Involved?
At the start of each menstrual cycle, multiple fluid filled sacs called follicles start to develop within the ovary. Within the follicle an egg develops, one follicle becomes dominant and ovulates an egg, the other follicles/eggs die prior to reaching maturity. In an egg freezing treatment cycle the ovaries are stimulated for approximately 11 days with hormone injections. These injections stimulate the growth of this group of developing follicles with the intention to collect multiple eggs during an egg collection procedure. Other medications are used to prevent ovulation prior to egg collection.
How Will The Eggs Be Collected?
Egg collection is performed using a vaginal ultrasound to see the follicles on the ovaries which are drained via a needle. The egg collection procedure is performed either under a general anaesthetic in hospital or in the Fertility Solutions clinic under local anaesthetic and a patient administered inhaled medication.
How Many Eggs Will I Need To Freeze?
The table below outlines the estimated number of eggs to freeze, by female age.
The number of eggs that may be collected in one treatment cycle is largely dependent on your individual egg reserve. This is determined through a blood test called Anti-Mullerian Hormone (AMH) as well as an antral follicle count (AFC) obtained via a pelvic ultrasound scan. Please see further information about this in the screening test section.
Of the total number of eggs collected during an egg collection, some may be immature and unsuitable for freezing. More than 1 treatment cycle is generally required to obtain the recommended number of eggs for freezing. The average number of cycles is 2 to 5 but will depend on the number of eggs collected from each cycle.
How Are Eggs Frozen & Stored?
All mature eggs collected undergo a freezing process (vitrification) and are stored in liquid nitrogen at Fertility Solutions.
How Long Can Eggs Be Stored?
Eggs can technically be stored indefinitely once frozen; however, the storage of eggs is regulated through the National Health and Medical Council’s (NHMRC) Ethical Guidelines along with clinic policy. These guidelines stipulate that it is not desirable to leave eggs stored indefinitely and that a clinic MUST have clear policies that limit and outline the storage duration.
Fertility Solutions policy is that eggs can be stored for a maximum of 15 years (which includes 10 years, plus a 5-year extension period). Please speak directly with our clinic if you have questions around the length of time eggs can be frozen and stored for your situation.
Your eggs will remain in storage, unless you request to use them for fertility treatment, indicate you no longer wish to store them (via signed consent) or in the event of your death (upon receipt of a death certificate).
What Is The Process Of Using Frozen Eggs?
Thawing Eggs
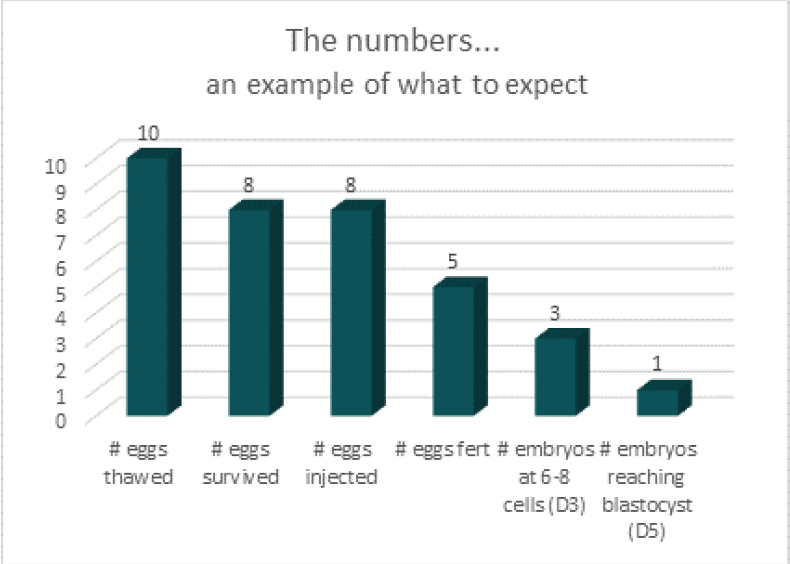
• Frozen eggs undergo a thawing process within the laboratory. It is expected that between 70% and 80% of frozen eggs survive upon thawing.
Inseminating Eggs & Fertilisation
• For successful fertilization to occur the thawed egg(s) need to have a single sperm injected directly into it, this procedure is known as Intra Cytoplasmic Sperm Injection (ICSI). Not every thawed egg will fertilise, however it is expected that approximately 70% of thawed oocytes injected with sperm will fertilise for a woman who froze eggs aged of 35 years or less.
Embryo Development
• Once an egg has been fertilised, an embryo develops. It is expected that one third of fertilised eggs, now embryos, will reach a stage of development (Blastocyst / Day 5 embryo) whereby, they can be frozen for future use.
Sperm quality and male age are also factors that impact fertilisation and embryo development.
What Are My Chances Of Achieving A Pregnancy?
The chance of a pregnancy is largely determined by female age at the time of freezing and the number of eggs frozen that convert to Day 5 (blastocyst) embryos. The chance of a pregnancy per embryo transfer for a woman using an embryo created from eggs collected at age 35 years is approximately 20-35%, this is similar to natural conception rates at this age.
What Can Go Wrong?
The process of egg freezing is continually being revised and updated. Sometimes things can go wrong. Some of these things are outlined below:
1. No eggs are collected at the egg collection procedure. The reported incidence of this complication happening is less than 5%.
2. The eggs collected are not mature and therefore may not be able to be suitable to inject in the future. This complication is not common and would be seen in less than 5% or cases.
3. None of the eggs frozen survive the thawing process. This complication is more likely to be seen when the number of eggs collected are low.
4. None of the thawed oocytes fertilise even though the sperm was injected into them. As with the above, this situation is more likely to occur when the numbers of eggs injected are low.
5. A pregnancy test is negative despite having an embryo transferred into the uterus.
6. A pregnancy may be confirmed but does not continue to develop i.e. miscarriage or ectopic pregnancy. This can also occur by natural conception.
7. A baby may be born with an abnormality. 2-3% of all babies born are reported to have an abnormality and is not necessarily related to having had fertility treatment.
It must be noted that all the above scenarios can occur under normal IVF procedures and with natural conception pregnancies.
Next Steps
A consultation with a specialist Gynaecologist who practices fertility treatment is recommended. You will need a referral from your General Practitioner (GP) to your specialist of choice.
You also have the option of discussing the various aspects of undergoing egg freezing treatment with a specialised fertility counsellor.
Screening Tests
Prior to commencing treatment with Fertility Solutions, you will be required to have mandatory screening tests. Other optional testing may also be considered. Some of these tests are performed to minimise the risk of transmission of infection from person to person, mother to baby or impact lab procedures. Others are to provide your doctor with essential information that helps them when planning your treatment.
Tests such as Hepatitis B & HIV do not provide a 100% guarantee that these viruses/infections are not present in the person being tested.
Your GP may be able to request some or all these tests to streamline the process for you. Some of the tests require an explanation before and after as to why they are offered along with the implications of an adverse result. Your GP may not feel comfortable in ordering them and request they be ordered by the Fertility Specialist at your first consultation.
WE SUGGEST YOU BOOK A LONGER CONSULTATION WITH YOUR GP IF YOU WANT THEM TO REQUEST THESE TESTS.
Essential (Mandatory) Tests
Baseline Pelvic Scan (Mandatory, only repeated every 12 months)
• This procedure assesses the female pelvis, uterus and ovaries for any obvious conditions that may impact upon fertility and should be performed in the first 10 days of menstrual cycle. The scan also reports uterine position, antral follicle count (potential ovarian egg reserve), and other information that is used to assist the nurse/doctor when performing treatment related procedures. The preference is that the scan is a detailed 3D pelvic ultrasound performed by a qualified sonographer. The 3D component of the ultrasound scan is the uterine and endometrial cavity assessment. This has been shown to be the most effective in detecting uterine problems when compared to 2D (black and white) USS, Sonohysterogram or Hysterosalingogram and is even considered a good alternative to Hysteroscopy and Laparoscopy (gold standard) for diagnosis of uterine anomalies (things outside the normal).
Pelvic USS should be repeated every 12 months as the incidence of polyps and fibroids increase as women age, especially from late 30’s onwards.
Anti-Mullerian Hormone Blood Test (AMH) also known as the egg timer test (Recommend repeating every 12 months, NOT Bulk Billed)
• Test can be done at any time of the month.
• AMH is a hormone produced by the ovaries by the developing follicles that contain eggs. The level of AMH in a woman’s blood is generally a good indicator of her ovarian reserve. Women are born with their lifetime supply of eggs, and these gradually decrease in both quality and quantity with age.
• You should NOT have this test while on the Oral Contraceptive Pill (OCP) or supplements containing Biotin (Vitamin B7, in most pre-conception multi-vitamins) as they can affect the accuracy of this test. It is recommended that you cease the OCP a full month prior to having this test and cease your supplements 3 days prior to having the test.
Baseline Female Hormones and Progesterone post ovulation Blood Tests (Bulk Billed)
• This blood test will provide your doctor with a baseline about how your body and ovaries may be functioning by assessing your Oestradiol (E2), Luteinising Hormone (LH), Progesterone (P4) and Follicle Stimulating Hormone (FSH) levels between day 2 and 4 of your period. In addition, a check on Progesterone level approximately 1 week prior to your period commencing, D21 for 28 day cycles, confirms if you are ovulating. These tests are used in conjunction with the AMH and Antral Follicle Count so your treatment can be individually tailored.
Vitamin D Blood Test
(Bulk Billed)
• Vitamin D deficiency is related to issues with egg quality, implantation and immune system function. Ideally your level should be 80 or greater. Optimised Vitamin D levels in pregnancy help reduce the risk of gestational diabetes and pre-eclampsia along with overall improved health outcomes for mothers and babies.
Infectious-communicable disease screening
Hepatitis B surface antigen Blood Test (Must be repeated every 2 years, Bulk Billed)
• Hepatitis B virus is an acute and chronic communicable disease that causes major liver disease.
• The virus it is excreted in various body fluids including blood, saliva, vaginal fluid, and breast milk. These fluids may be highly infectious.
• Adults who have hepatitis B may have no symptoms.
• There is a 90% chance of the infection being transferred to baby if they are not treated at birth if the mother already has the infection.
• Hep B Vaccination is safe to receive during pregnancy for mothers.
Hepatitis C antibody Blood Test (Must be repeated every 2 years, Bulk Billed)
• The hepatitis C virus which is transmitted through blood-to-blood contact.
• If left untreated, it can lead to liver damage, cirrhosis, and liver cancer.
• If the mother is infectious, treatment is not recommended during pregnancy due to potential birth defects.
HIV 1 & 2 Blood Test (Must be repeated every 2 years, Bulk Billed)
• Human immunodeficiency virus (HIV) is a blood-borne infection that is initially asymptomatic but involves gradual compromise of immune function, eventually leading to acquired immunodeficiency syndrome (AIDS).
• It is transmitted via semen, vaginal fluid, blood, and anal mucus. It can also be transmitted to a baby during pregnancy, at birth or through breastfeeding.
Syphilis Blood Test (Must be repeated every 2 years, Bulk Billed)
• Syphilis is a communicable infection caused by a bacterium. • Syphilis in pregnancy can be safely treated with antibiotics, which can prevent these complications.
• Untreated syphilis during pregnancy is associated with stillbirth and foetal loss, preterm birth, neonatal death, low birthweight, and congenital syphilis.
CMV Serology Blood Test (Must be repeated every 2 years, Bulk Billed)
• Cytomegalovirus is a member of the herpes virus family transmitted by contact with saliva, urine or genital secretions.
• Most people who acquire the virus after birth experience few or no symptoms.
• Cytomegalovirus remains dormant after primary infection and may become active again particularly during times of compromised immunity, including pregnancy.
• Congenital cytomegalovirus (infection of the baby that is present at birth), is the most frequent infectious cause of newborn disability. Spread of infection from mother to child may occur across the placenta resulting in congenital infection in the baby.
• Effects of CMV infection during pregnancy include late miscarriage, stillbirth and growth restriction.
• Approximately 10% of babies infected with cytomegalovirus in utero will have symptoms at birth and are at high risk of developing hearing loss (35%) or intellectual deficits (up to 60%), other neurological disabilities (epilepsy and cerebral palsy) or death (4%).
HTLV type I & II Serology Blood Test (Must be repeated every 2 years, Bulk Billed)
• The Human T-cell lymphotropic viruses (HTLV) are part of the same group of virus’s as human immunodeficiency viruses (HIV).
• HTLV-1 is transmitted from mother to child mainly through breast feeding. About 20-50% of the babies born to infected mothers will become carriers. Other ways the disease is passed on are by blood transfusion (if the blood is not screened for HTLV-1), sexual intercourse and by sharing contaminated needles.
Chlamydia/Gonorrhoea Urine Test (Must be repeated every 2 years, Bulk Billed)
• Chlamydia/gonorrhoea are communicable infections (sexually transmitted) caused by a bacterium.
• They can be contracted through oral, genital, or anal sex.
• In pregnancy, untreated Chlamydia/Gonorrhoea, can cause pregnancy and neonatal complications, i.e. pelvic inflammatory disease (PID), neonatal conjunctivitis which can lead to blindness if untreated, pneumonia, miscarriage, or stillbirth.
If you are in an intimate relationship (casual or long term) your partner is also required to have these infectious-communicable disease screening tests.
Optional Testing
General health checks such as investigations for thyroid function, iron, diabetes, coeliac disease and other health related conditions as deemed necessary by your GP or specialist are also highly recommended.
References
References: R.H. Goldman, C. Racowsky, L.V. Farland, S. Munné, L. Ribustello, J.H. Fox, Predicting the likelihood of live birth for elective oocyte cryopreservation: a counseling tool for physicians and patients, Human Reproduction, Volume 32, Issue 4, April 2017, Pages 853–859, https://doi.org/10.1093/humrep/dex008