An IVF (in vitro fertilisation) cycle is defined as one complete round of IVF treatment consisting of several steps which result in pregnancy, if successful. The steps that are involved in an IVF cycle are dependent upon the clinic that you are visiting, the specialist you are working with, and the treatment they believe is correct for your personal situation. For the majority of fertility clinics in Australia, part of the process includes a number of screening tests that couples have to undertake before they can even embark upon any form of treatment.
IVF Process
Step 1. Ovarian Stimulation
Once the screening tests have been done, the first step of an IVF cycle is called ovarian stimulation and simply means stimulating the ovaries to help them produce eggs. Normally, a woman’s ovary produces one egg per month, but with an IVF cycle, we are trying to get the ovaries to produce two, three, or more eggs per each ovary.
In the past, IVF clinics used to look at stimulating women, so that their ovaries produced in excess of 10 or more eggs per ovary. But as we have become more educated in the process, we are now learning that “less is best,” and as a result, many clinics are working toward this goal. The aim is to get single figure numbers between both the ovaries, so that the total number of eggs produced is between 8-12.
How is ovarian stimulation performed?
The way ovarian stimulation is done is the woman is given medication. This medication is referred to as “follicle-stimulating hormones” and is very similar to the hormone the brain produces naturally in females every month to stimulate their ovaries to produce one egg.

The medication is given through injection once per day. Women may give themselves the injection, or their partners can administer it for them.
How many days do the injections last?
Usually, injections last between 8 – 12 days. Everyone is different, and whilst we have a fairly broad algorithm that we use to determine what may be the appropriate dose for each person, the amount of medication needed varies from one woman to the next. The dosage used on one lady, may be totally ineffective or over effective for another woman.
How do you monitor the success of the injections?
We monitor the process by doing blood tests and ultrasound scans to see how the ovaries are responding to the medication. When we are doing the ultrasound scans, which are usually trans-vaginal, we are actually looking at the follicles on the ovary.
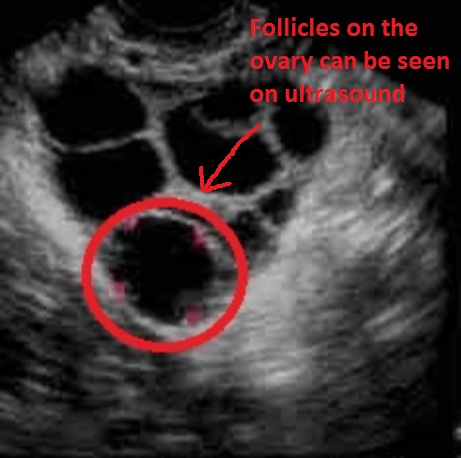
There are often two or more ultrasound scans in one IVF cycle.
How successful are the injections in producing follicles?
There are three things that can happen during the stimulation phase of the ovaries: There can be a normal response, there can be an under response, and there can be an over response.
Normal Response: For 80-90% of women, the medication dosage they are given is just right and she is able to proceed right through to the egg collection procedure.
Under Response: Occasionally, we’ll find that the woman hasn’t responded particularly well to the medication she has been given, and at that stage, there are a couple of options.
- Stop this IVF Cycle. A woman/couple can choose not to pursue the IVF cycle that month and stop the injections. This allows their ovaries to go back to normal, which might take a month or so. They can commence their IVF cycle on a higher dose of medication in a subsequent month.
- Artificial Insemination. For some women, if there is not a large number of follicles on the ovaries, (only one or two follicles), they may elect to transfer their cycle from an IVF cycle into an artificial insemination cycle. So at least they have an opportunity for pregnancy that month. (Of course, there has to be pipe tubes or the tubes have to be open, and the sperm has to be of a certain quality to be suitable for using artificial insemination cycles.)
- Continue this IVF Cycle. The other option is where the patient decides to still go ahead with the egg collection procedure even knowing they have only got perhaps one or two follicles.
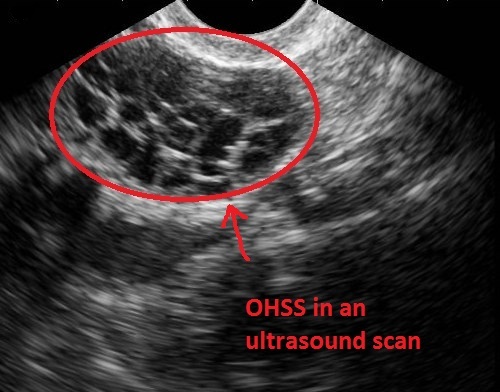
Over Response: This is where we see women developing a fairly serious condition called ovarian hyperstimulation syndrome or OHSS. And in this situation, it can be life threatening. Women have died throughout the world because of this particular condition.
But it’s important to say that it’s something that can be monitored very closely, and actually if it’s acted upon very quickly, it shouldn’t result in any form of a life threatening situation. What happens is the ovaries become over-responsive to the medication, and if you can visualize like a “bunch of grapes,” that’s what the ovaries look like, and each one of those little grapes is actually a potential egg.
Step 2. Egg Collection
When it’s determined by the clinic or the doctor that the follicles are of a size that they contain eggs which are mature and suitable for fertilization it’s time to perform the egg collection procedure. People often refer to the egg collection procedure as an “egg pickup”. Medically, it’s called an “oocyte pickup” because the medical name for an egg is an oocyte.
The Trigger Injection
In order to initiate the egg collection procedure, the woman needs to have a trigger injection. This is an injection that’s administered by the female again or perhaps her partner, and that is usually administered into the tummy about 36 hours prior to the scheduled egg collection procedure. This injection is designed in such a way that it will help the eggs that are growing undergo the final maturing process, and that final maturing process enables that egg, once it’s collected, to potentially fertilize. Without the trigger injection, the fertilization process would probably not take place.
Where does the egg collection procedure take place?
The actual location used for the egg collection procedure varies from clinic to clinic, but it’s usually considered to be a day surgery procedure where women are admitted into a hospital. Some IVF clinics have their own day surgery facility on site.
Is sedation required during the egg collection procedure?
The egg collection process is an outpatient procedure and isn’t necessarily that painful for the woman, although perhaps it’s a psychological thing, because some women choose to have some form of a sedative or an anesthetic.
Women who choose to be anesthetized receive oral sedation, such as valium, or a local anesthetic inserted into the vaginal walls. But more commonly, only a light sedation is given. In some instances, the women have a full general anesthetic.
What is the actual egg collection procedure like?
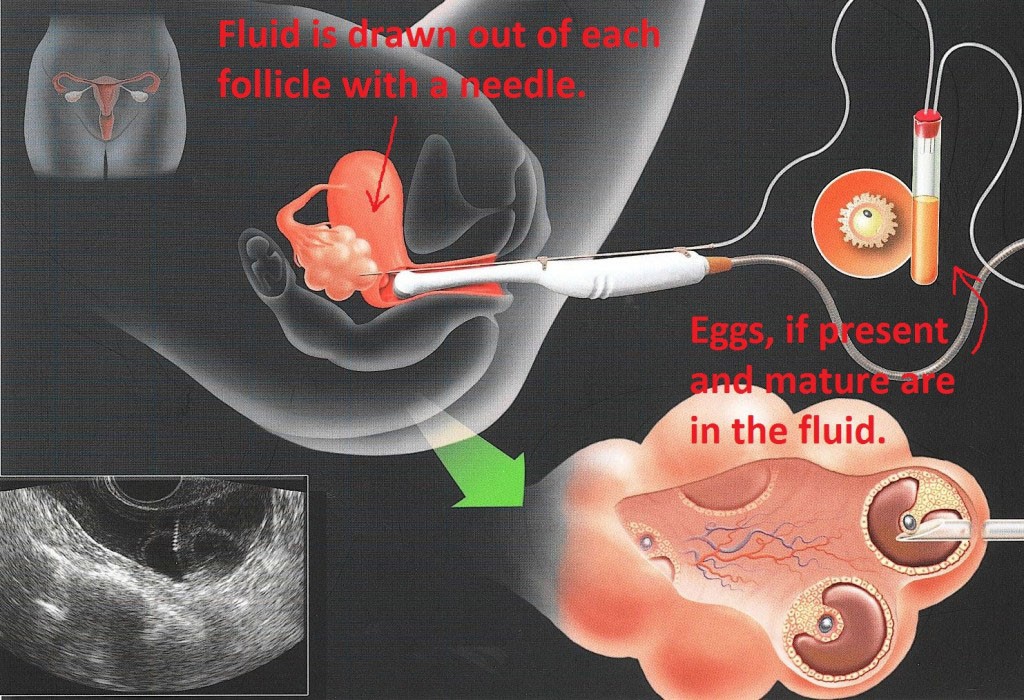
An ultrasound probe is inserted into the vagina and a very fine needle is inserted alongside the ultrasound scanning probe. The needle can be visualized by the doctor on the ultrasound machine screen.
As the needle is advanced into the vagina, it actually penetrates through the vaginal walls and is guided through to where the ovaries are, and then the needle is inserted into each one of the little follicles that the doctor can see on the ultrasound screen.
The actual needle has a test tube attached to it. Subsequent to the needle being inserted into the follicle, the negative pressure creates a suction which throws the fluid out from the follicle and along with it, if the egg is mature or there is an egg present in that follicle, the egg would come away in that follicle fluid.
When the procedure is completed, there are no stitches, as it’s just a very fine little traversing through the vaginal wall.
How long does the egg collection procedure take?
More often than not, the actual procedure only takes about 20 minutes, depending upon the number of follicles present. Most women are right to leave the hospital or the day surgery within 1 to 5 hours of having the procedure.
They can return to work the same day if they haven’t had any form of anesthesia. If they had some form of anesthesia, they are okay to return to work the next day after their egg collection procedure.
Once the eggs are extracted, do you already know if they are mature enough to be able to be fertilised?
We don’t know. We have to test them. We can use the size of the follicles as a guide, but the real test is actually examining the eggs themselves. After the egg is collected in the follicle fluid into a test tube, our scientists then examine the follicle fluid looking for the presence of eggs.

But the real test occurs after the sperm has actually been placed with the egg. The sperm relays a chemical that strips away that cotton wool covering around the egg, allowing the scientist to visualize the egg in its entirety. At that point, the maturity of the egg can be determined. Having said that, usually, that’s not until about 18 hours after the egg has been inseminated with sperm.
If it turns out that the egg is not mature, then there is nothing that can be done about it. There is nothing that we have at this point in time with our technology that can assist the maturity of the egg to enable it to fertilize in a subsequent day or two’s time. There is nothing that we can do.
How soon after mature eggs are collected are they inseminated with sperm?
Usually, the egg collection procedure is scheduled as a morning procedure. The partner, meanwhile, produces his sperm sample usually a couple of hours after the egg collection has taken place. (Or if the sperm is being donated, the donor sperm is produced at that time, so it is ready for the egg just to be inseminated with it.)
The actual insemination of the egg with the sperm takes place between four and six hours after the egg collection, depending upon the workload in the laboratory.
When the sperm is placed with the egg, it’s about 18 hours after the sperm has been inseminated with the eggs – assuming this is just straightforward IVF because, of course, there’s another means of fertilisation which is called ICSI, which is Intracytoplasmic Sperm Injection – that the scientists are able to identify whether fertilisation has taken place. And that leads to step 3 and that is fertilisation.
Step 3. Fertilisation
What the scientists are looking for are two little depressions What the scientists are looking for are two little depressions that actually occur on the egg, and those two little circular depressions are called pronuclei.
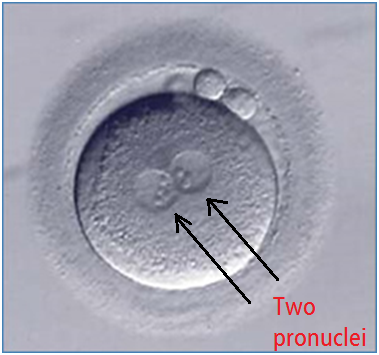
One of those little circular depressions represents one of the sperm’s chromosomes and the other one is the egg’s chromosome. Both of those little circular depressions after a period of time will merge together, and that’s when you actually have the aligning of both of the chromosome’s material and the egg starts to divide. First it divides into two cells and then slowly but surely it will divide into three cells, four cells, six cells, and so on.
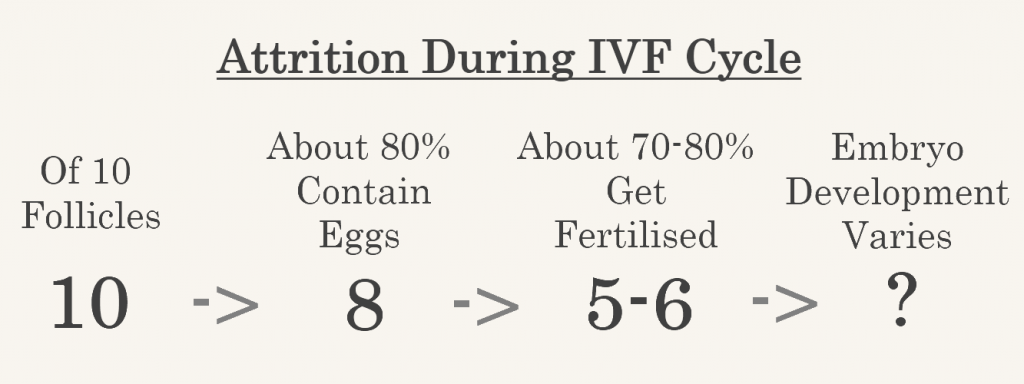
It’s important to say that when the sperm is placed beside the egg and fertilisation is still occurring in the laboratory, it’s occurring in a natural form. We would expect around 70-80% of mature eggs to get fertilised.
Therefore, you can see why it’s important when ovarian stimulation is taking place that we are trying to get not a huge number of eggs but not a really low number of eggs either because there is a slow attrition rate as you move through the process. The first attrition rate is the number of eggs that you collect from the follicles, and then the second attrition rate will be the number of eggs that are collected that subsequently fertilise.
After the fertilisation takes place, unfortunately, humans aren’t particularly efficient in procreation. The eggs, whilst they may have fertilised, may not continue to develop at the right rate. Sometimes they just fertilise and then stop their development; sometimes they are divided into four cells and then stop their development, for any number of reasons. So, there is not necessarily a guarantee that – despite fertilisation – a fertilised egg will continue to grow at what would be the expected rate of growth for what we would now call an embryo.
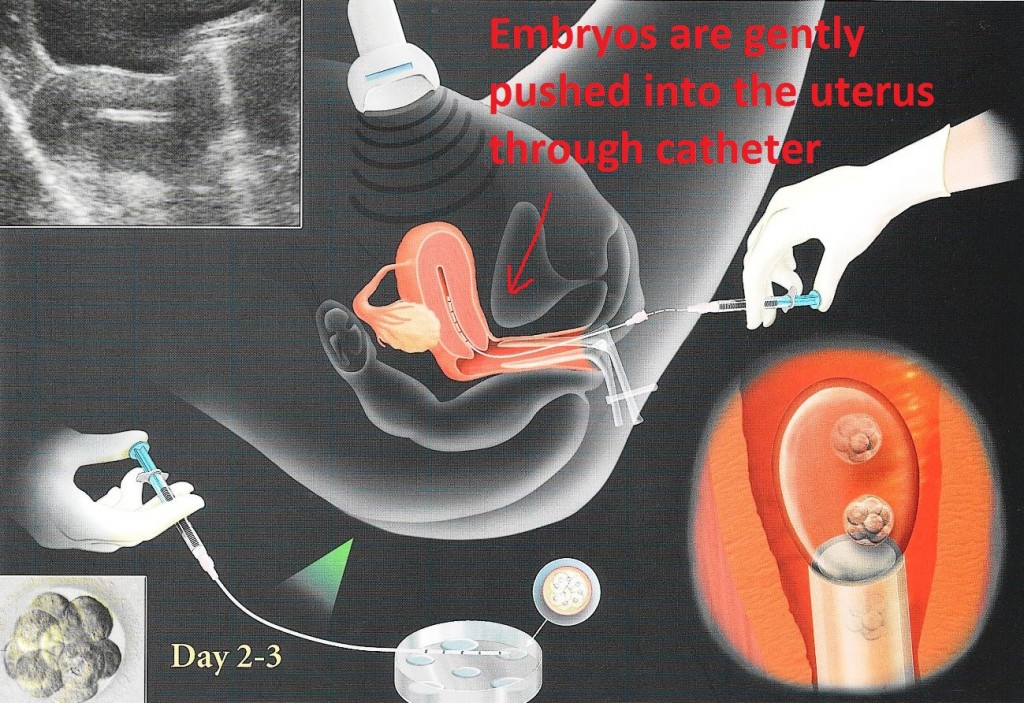
Embryo transfer usually occurs between day two and day five after fertilisation, depending on the clinic. So if an egg collection took place today, tomorrow you would know how many have fertilised, and then the next date at the earliest, the embryo would be transferred to the woman.
Sometimes an embryo (or embryos) are cultured on to what we call a blastocyst, which is essentially an embryo on about day five to six of life when it’s just a little ball of cells. If an embryo reaches that stage of development, there is a higher chance – but not a guarantee – that that embryo could result in a pregnancy.
It’s quite common to find embryos do not make the day five progression. Many embryos will stop development before that, and therefore it’s safe to assume that those embryos themselves, even if they had been transferred back to the female earlier in the process would not have resulted in a pregnancy.
The embryo transfer takes place, again, as an outpatient procedure. It’s usually done at the clinic or perhaps in a day surgery center. For women, the procedure is similar to having a pap smear. No medication is required.
How is the actual embryo transfer procedure performed?
The cervix or the neck of the womb has to be visualized. In order for that to happen, a speculum has to be inserted into the vagina, and the doctor or nurse performing the embryo transfer passes a very fine little catheter through the neck of the womb and into the womb itself.
There is no pain or discomfort. Some women actually describe the sensation – if they feel anything at all – as like having a little bit of a period cramp. That’s generally as far as the actual discomfort goes.
Once the catheter is inside the womb, the scientist is informed and takes the embryo or embryos out of the incubator, so they can be transferred into the womb. (Up until this point in time, it’s very important not to disturb the embryos too frequently. They are very sensitive to temperature, light, humidity, and other changes, so leaving them in the incubator for as long as possible and disturbing them as little as possible is important.)
Depending upon the age of the embryo when it was transferred, it could move around inside the uterus looking for a suitable place to implant for several days.
It’s essentially been placed into a big sponge and it doesn’t immediately implant. It will actually “putter around” inside the uterus looking for the place that’s just right for it to implant. Of course, there are going to be a number of embryos that for a variety of reasons don’t reach the implantation state, so they just never end up resulting in a pregnancy.
What happens immediately after the embryo transfer?
Many women are concerned about having to lie flat for a number of hours or perhaps drive home with their legs sitting outside the windows of the car, but the reality is that the embryo has been absorbed into this sponge environment, and they don’t fall out!
Some women feel comfortable lying flat perhaps a few minutes after the embryo transfer, but there is a lot of data out there that suggests there is no benefit in doing this. It’s actually just getting straight up and going home or going to the toilet or whatever they need to do after the embryo transfer is complete.
Then they just try to go home and resume their life as normal as possible waiting for their next appointment, to test for pregnancy.
Step 5. Embryo Freezing
Cryopreservation is a term used to describe the freezing of biological material for future use. However, it is more commonly referred to as freezing or vitrification. Vitrification is a rapidly developing technology used for freezing eggs or embryos that is fast and highly effective in providing high survival rates, due to the low risk of damage to cells in an embryo from ice crystal formation. This technique was introduced into Fertility Solutions in 2011. Prior to this (or at least since the 1980’s), embryo cryopreservation was achieved through a method referred to as Slow Freezing. This technique is not as successful as vitrification, as the slower transfer of cryoprotectant into the cells of an embryo, and gradual reduction in temperature resulted in a higher chance of ice crystal formation.
What Happens During Embryo Cryopreservation?
Freezing/vitrification involves placing the embryos in a cryoprotectant fluid that protects them during the freezing process. The degree of success of the freezing and thawing process comes from the effective removal of water from the cells. When water freezes it expands and forms ice crystals, which are very destructive to the delicate cellular components. Cryoprotectants have been specifically designed to get deep inside the cells and replace water, this allows the embryos to better withstand the dramatic reduction in temperature. The presence of cryoprotectant, coupled with the speed of freezing in vitrification, means that crystals do not get a chance to form, instead the fluid within the cells instantaneously solidifies into a solid glass-like structure, preserving the internal cellular components. Generally, you can expect that roughly 90-95% of embryos frozen will survive the vitrification/warming process. Therefore, if you only have one embryo in storage there is a chance, albeit small, that this may not survive the process and as a result, you may not have an embryo suitable for transfer.
Embryo Cryopreservation is an important process used in Assisted Reproductive Technologies (ART). It allows any additional ‘good-quality’ embryos present at the end of a fresh stimulated cycle to be stored. This gives a patient further attempts of pregnancy without having to undergo another stimulated cycle. Embryo vitrification is routinely performed throughout Australia and the world, and there have been many babies born through this technique. Given embryo cryopreservation has seen such improvements in the survival of excess embryos, and more research has been conducted into the impact of stimulation drugs on the endometrium, the pregnancy rates using frozen embryos are comparable if not better than that of fresh embryos. The goal of embryo freezing is to give patients the same, if not better, chance of conceiving a child without having to undergo another fresh stimulated cycle.
Why Don’t All Embryos Get Frozen?
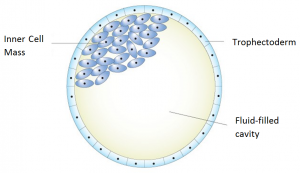
Embryos left in culture are evaluated at days 5 and 6 for blastocyst quality and development. There are 3 distinct parts to a blastocyst – the two cell types (Inner Cell Mass & Trophectoderm) and the fluid cavity. As development of the blastocyst progresses, the two cell types divide and the fluid-filled cavity enlarges. With continued blastocyst development the embryo expands, the zona pellucida (or shell) thins, and the embryo ‘hatches’. Blastocyst implantation into the lining of the uterus can then begin.
Unfortunately not all embryos will continue to grow to the blastocyst stage, and similarly will not survive the process of being frozen and thawed. Therefore, only embryos of ‘good-quality’ will be considered for freezing. At Fertility Solutions this means that we will only freeze embryos on day 5/6 of development to give you the best chance of pregnancy. It is expected that for an embryo to be frozen on day 5, that it has reached at least blastocyst stage and has an ICM and trophectoderm which is graded A or B quality. [For more information about grading of embryos, please see our article: Choosing Embryos for Freezing or Transfer]. This is because these embryos have a higher chance of survival and therefore are thought to be more viable when trying to achieve a pregnancy.
How Long Can Embryos be Frozen and Stored?
Given they are stored in the optimal conditions, frozen embryos can remain in storage indeterminately. However, all IVF clinics within Australia must be accredited by the Fertility Society of Australia, which requires compliance with the National Health and Medical Research Council (NHMRC) Ethical Guidelines. Part of these guidelines deal with the issue of embryo storage and as such, recommend that embryos are not stored indefinitely.
Therefore Fertility Solutions provides embryo storage for 5 years with the option to renew for a further 5 years, equating to a maximum period of 10 years storage.
There are many complex ethical, religious and emotive issues associated with embryo storage, embryo donation and allowing embryos to succumb. The existence of diverse views on when life begins, and the experience and outcomes of an individual/couples fertility treatment will impact on the decision-making process once the permitted timeframe for embryo storage has been reached. There are options regarding the fate of embryos at this time. One may be embryo donation, where the embryo(s) are offered to another couple so that they too may be able to have a family. Another option is to allow any embryo(s) remaining in storage to respectfully succumb, which involves removing the embryo(s) out of storage and allowing to thaw.
If you would like more information on the embryo freezing step of the IVF process, please phone (07) 5478 2482 and speak with a Scientist.
Step 6. Pregnancy Test
Approximately two weeks after the embryo transfer, the woman will either have a urine test or a blood test to signify whether they are pregnant or not. This is the final step in determining whether an IVF cycle has been successful or unsuccessful.
If you have any questions about your IVF Cycle, you are encouraged to contact your specialist, nurse or a scientist.
Why Do I Have Less Eggs Than Follicles and Even Fewer Embryos?
This is a common question asked by patients during the IVF Process. Click here for more information on our blog page.
IVF Treatment Options at Fertility Solutions
To download a copy of our IVF Treatment Options, click here.