You have just been told that you could have endometriosis – now what?
What is Endometriosis?
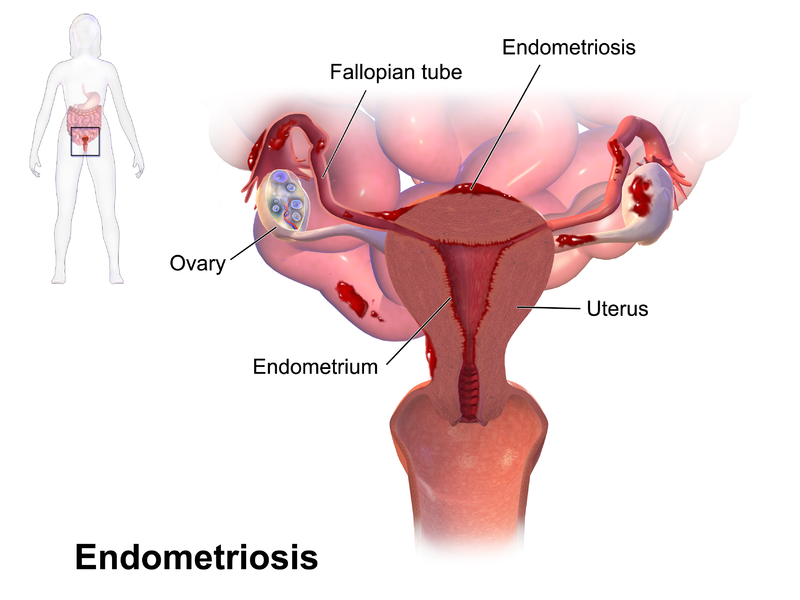
Endometriosis is a common and often painful condition that affects approximately 10 – 15 per cent of women. It occurs when the lining of the uterus/womb (called the endometrium) grows outside the uterus. The displaced tissue commonly grows on the uterine (fallopian) tubes, the ovaries or the tissue lining the pelvis (called the peritoneum), or on the bladder or bowel. How this happens is really unknown although there are many theories. Below are a few of the more common ones:
- Retrograde Menstruation – The uterus is always contracting in a forward manner – with the contraction starting at the top of the uterus, making its way, like a roller coaster, down to the bottom of the uterus and cervi. This is how the lining of the uterus is shed when you get your period. Retrograde menstruation is when the uterus’s roller coaster contractions go backwards from the cervix to the top of the uterus, which results in the lining of the uterus going out the tubes and deposited in the pelvis. It then continues to grow and act like the lining inside the uterus – bleeding every month and because there is nowhere for the blood to go (like out the vagina), this can cause pain, bloating and scar tissue. Why this happens, no one knows!
- Hereditary Influences – It is thought that endometriosis can be passed from one generation to the next and research has shown that women who get the condition come from all different ethnicities.
- Blood Stream and Lymphatics – Endometriosis cells are thought to find their way into the bloodstream or lymphatic system (the tubes, glands and organs that are part of the body’s defense against infection). This could explain how, in very rare cases, the cells are found in remote places such as the eyes or brain. Again, the process behind this theory is not known.
- Cells Disruption – It is thought that when a baby is developing that the body gets confused and some of the cells lining the uterus (endometrial cells) are displaced in other areas such as the pelvis.
Endometriosis Questions You May Have
Having been told that you could have endometriosis can be very confronting for a patient. What does this mean? You have a million questions that you want answers to:
- Will it affect my life?
- Will it affect me having babies?
- Does this mean I will get sick later in life?
- Which doctor should I go to?
- Do I need to see a doctor just yet, unless I’m having difficulty getting pregnant?
- Should I see a gynaecologist, an obstetrician or a fertility specialist and what treatment is available?
Often, after seeing your GP, the next doctor you will see is a gynaecologist with or without a fertility interest. Sometimes doctors will advise a laparoscopy (key hole surgery) to see if you have the condition, but is this the first treatment option?
Endometriosis Symptoms
You should do your own research if your doctor has suggested a laparoscopy just to “see”, especially if you do not have any symptoms of endometriosis such as:
- Pain just before and during your period, during or after sex, pain when going to the toilet – bowels or bladder, severe ovulation pain that can spread down your legs, abdominal, pelvic; or back pain that stops you doing the normal things in life.
- Bleeding usually heavy (can include clots), a period that lasts a long time i.e. 10 days, or spotting before your period.
- Reduced fertility, that is, trying for a pregnancy for 12 months (if you are under 35) or 6 months (if you are over 35) and no success.
- Heavy bleeding, with or without clots.
- Irregular bleeding with or without a regular cycle.
- Prolonged bleeding.
- Premenstrual spotting.
It is important that patients realise just because a laparoscopy allows the doctor to see if there is any visible endometriosis present (not all endometriosis is visible) and treat the disease, unfortunately endometriosis lesions, even once surgery has been performed, often come back as early as 6 – 12 months after your operation.
Endometriosis and Infertility
Often patients are led to believe that removing the disease spots will improve their fertility and allow them to have a baby, and as such, they agree to the surgery – especially if they also have pelvic pain because of their endometriosis. However, there are two major problems with this way of thinking.
First, there is no evidence that treating mild endometriosis improves fertility. It is not uncommon for a woman to have had a laparoscopy for other reasons and the doctor incidentally finds endometriosis that was not causing any apparent problems. It’s important to understand that a lot of fertile women who have had no problems having babies have endometriosis.
Secondly, the surgical removal of endometriosis can itself actually result in fertility challenges. While removing chocolate cysts (endometriosis deposits on the ovaries), the doctor also often ends up removing healthy, normal ovarian tissue. This further reduces ovarian reserve and ability to produce eggs.
The extent of endometriosis and the appropriate treatment is a controversial issue. Mild endometriosis most likely does not affect fertility at all – and can be left alone. Severe endometriosis is a more complex issue, and management needs to be individualised, based on what your goals are. For information on degree of severity refer to https://www.asrm.org/Endometriosis_booklet/.
Endometriosis Treatment
The decision to treat endometriosis with a laparoscopy presents the patient with a lot of difficulties. To assist in the decision making process, consider the following important points:
- Your age
- Your ovarian reserve
- Whether you are trying to have a baby or not
- The extent of your disease
- Whether or not you also have additional symptoms such as pain, for which you need relief
Your Age
If you are over the age of 35 and under 40 and have not started or completed your family – time is of the essence for you. It is important that you consider more aggressive fertility treatment options in order to get pregnant as soon as possible. This is where IVF may be able to help. The good thing about IVF is that not only does it maximise the chances of you becoming pregnant – once you get pregnant, your disease will reduce in severity, and you will be pain free. Now that’s a bonus!
However, if getting pregnant is your primary goal, and the diagnosis of endometriosis was an incidental finding (for example, when it was diagnosed during a baseline vaginal ultrasound scan), then your priority should be on maximising your chances of having a baby quickly by using assisted reproductive technology. Either way, the message is you don’t have time to wait, so do everything you can to become pregnant in the shortest possible time.
If your situation is such that you have incapacitating symptoms which need to be treated (for example, pain during or after sex), then a laparoscopy may be your first choice, as it may allow the doctor to effectively remove or reduce these painful lesions, giving you temporary relief.
Ovarian Reserve
Perhaps one of the most important things to establish is your ovarian reserve. Knowing this will help direct the course of action that is most appropriate for your situation.
Women are born with all of the eggs that they will ever have, and they lose them constantly throughout life until menopause, when none remain. Unfortunately, there is no current reliable test that would tell us how many eggs a woman has remaining at any point in time – as well as telling us about the quality of those eggs. The term “ovarian reserve” is used often in reproductive medicine and is an estimate of the “reserve of the woman’s ovaries” – remaining egg supply – to be able to make babies in the future. In short, a woman’s ovarian reserve is her remaining fertility potential.
It is important if your doctor does not offer you this test that you ask them to check your ovarian function, before proceeding further. This needs to be done both by doing an antral follicle count (AFC during a pelvic ultrasound scan), and by testing your blood Anti Mullerian Hormone (AMH) levels.
AFC
Antral follicles are small follicles (about 2-8 mm in diameter) that can be seen, counted and measured – with ultrasound. Antral follicles are also referred to as resting follicles.
AMH
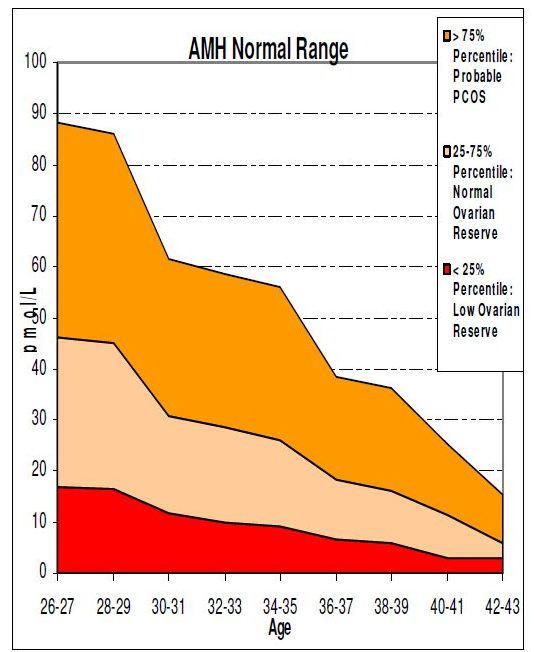
This is the most recent test that is being used to assess ovarian reserve. AMH is a hormone produced by the ovaries by the developing follicles that contain eggs. It is now thought that it could be an indication of the number of eggs being produced during a monthly cycle. It can be measured by a blood test at any time during the month although women taking the oral contraceptive pill who have an AMH result indicating reduced ovarian reserve should consider having the test repeated after a full month off the contraceptive pill.
It is extremely important to consider your AMH result in conjunction with your age (see chart below).
If you have a normal AFC (15 – 30 follicles between both ovaries) and a normal AMH level for your age (14 – 30 pmol/l), you can elect to have surgery.
However, if you have a low ovarian reserve for your age, then you need to be cautious about opting for surgery, as this can further damage your ovarian reserve. You might want to consider going straight for IVF treatment.
The problem with surgery is that not only are the results unpredictable, it can actually end up wasting valuable time in which you could be trying for a pregnancy. After the surgery, doctors often put patients on medical therapy for 2 – 6 months (such as Zoladex implants of Synarel nasal spray) to allow the endometrial lesions to heal. These medications work by suppressing any endometriosis deposits that may still be in the pelvis. Often after the 2 – 6 months have elapsed, patients are told to try for a pregnancy naturally for another six months. By the time the patient has waited 8 – 12 months, often the endometriosis is back again.
The rule is simple – think not just about the disease and its diagnosis, but about your age, your ovarian reserve and your final goal – either to have a baby or to be symptom free. If your primary aim is not to “treat the endometriosis”, but to have a baby, then it may well be better to consider bypassing the problem and having fertility treatment rather than trying to fix it with surgery. Food for thought!